6 - COMPARISON BETWEEN OSSEOINTEGRATED IMPLANTOLOGY AND ITALIAN SCHOOL IMPLANTOLOGY
PREMISE
The average implant of the osseointegrated school is a large volume implant and requires the removal of large quantities of bone. The average implant of the Italian school is an implant that can be of large diameter, compared to the corresponding size of the other school, but occupies a small volume and requires the removal of minimal quantities of bone.
LET'S PROCEED TO THE COMPARISON
It takes a moment of patience; the details are many and the choices you make have important consequences.
THEY ARE NOT CHALLENGE and it is a real shame that some implants are defined as osseointegrated even if they are still contained in the original packaging. Because maybe all of them will integrate or maybe not, but only after being inserted and after a reasonable amount of time spent while the patient uses them under normal conditions. The battle for osseointegration is waged and won only after several years have passed. Because, among other things, osseointegration may not be forever .......
CONSEQUENCES DURING THE DESIGN PHASE
In the design, the large volume implant requires that adequate safety spaces be left with respect to contiguous sensitive anatomical structures: dental roots, cortices, vascular-nerve fascicles, maxillary and nasal sinuses, due to the need to remove large volumes of bone .
It can therefore only be used with mandibles and maxillaries of adequate size in the three planes (class A bone of the Mish classification on the available bone.
All those patients are therefore excluded who, for various reasons, are less skeletally gifted; they will have to face a much more demanding path from a surgical, biological, human and economic point of view. Why ?
As Mish says in the classification of the available bone, in classes B and C it is necessary to regularize the areas of the thinnest ridge with osteoplastics extended even from sixth to sixth, in total edentulism, to recover superficial areas suitable for containing implants with a suitable diameter.
This bone removal weakens the structure of the jaw; and it is precisely the knife-blade cortices of the crest that are most opposed to the flexion of the mandible, and have greater density, which are affected by these surgical maneuvers.
But they could and should be saved and used. Which is what is done with the technique of the Italian school. Because having his implants with a neck of only 2 mm in diameter, they accept to be inserted without the need for osteoplasty.
As an alternative to osteoplasty, Misch prescribes ridge augmentation by bone apposition to be taken from intraoral, extraoral sites, from banks appointed to collect homologous and heterologous bone, or with natural or synthetic bone substitutes.
Surgical interventions are therefore required before implant surgery with their own times, methods of execution, risks, complications and variable outcomes to be taken into consideration.
CONSEQUENCES DURING THE INSERTION
A set of drills of increasing diameter and length is usually used to place an 'osseointegrated' implant. As the size of the drill increases, the risk of bone overheating increases, with the need to use irrigation external or internal to the drill, whose effectiveness is variable; Continuous back and forth are also required to minimize this overheating and to free the cutter from bone chips.
Proceeding at the recommended speeds between 400 and 600 rpm, but also occurs at significantly lower speeds, the gyroscopic effect occurs which, in the absence of a more than good stability of the patient's head and the operator's hand, or if there is a slight variation in the inclination of the cutter, causing sudden movements of the cutter itself with consequent risks of damage to nearby structures.
For this reason it is always recommended to detach the mucous membranes and the periosteum.
On the contrary, with a Tramonte implant, the flap is not foreseen except in exceptional cases.
Let's go back to the 'osseointegrated' technique.
The final dimension and depth of the neoalveolus are reached in successive phases, by inserting drills of increasing diameter and with stops at progressive depths.
It is almost imperative to proceed using surgical templates; in addition to guiding the insertion according to the logic of prosthetically guided surgery, they significantly reduce the sudden flapping of the drills.
The fixity and precision of the template anchors are essential, and complicate the painstaking work due to the presence of the unglued edges. Often a surgical guide that is not well fixed or not well positioned has led to incorrect perforations with consequent complications affecting the implanted area.
A reduced opening of the buccal rim reduces the chances of intervening in the posterior areas.
A perforation of the vestibular or lingual cortex makes the use of reparative membranes essential, with results to be verified over time.
Routing in these conditions close to a root, an artery, a vein or worse, a nerve trunk, causes great damage and is absolutely to be avoided. In fact the guidelines indicate in 2 mm. the distance from nearby sensitive structures.
The action of a helical cutter has a corkscrew effect and the most imprudent operators may find themselves with the inferior alveolar nerve twisted to the cutter that has torn it from its seat and consequent criminal and civil claim for damages.
Thus the perforation of the lingual cortices can induce the laceration of vessels of the buccal floor with extravasations which, even if not important, are still clearly visible and annoying.
Similarly, the periodontium of the neighboring tooth can be severely torn with imaginable consequences. If there is no mucoperiosteal flap, in case of perforation of the vestibular or lingual / palatal cortex, the damage can transport connective cells into the bone context, which can cause the loss of so-called osseointegration during the reparative phase.
Similarly, the bur can tear the Schneider's membrane causing a positive Valsalva maneuver and sinus problems.
For all these reasons, using only small diameter cutters is highly preferable and safe.
CONSEQUENCES DURING AND AFTER HEALING
How much bone can I sacrifice?
It cannot be forgotten according to what Dr. Misch and in other places the dott. Chiapasco, that a volume of 1mm of bone surrounding the perforation undergoes necrosis in the following weeks, making it mandatory to rest the implant pending bone reconstruction, given the loss of initial mechanical stability, after the first two weeks.
On p. 234 of his book Misch states: 'As shown in fig. 17.18, about one millimeter of compact bone near the wound dies after surgery, regardless of the quality of the surgical techniques used.
Let's do the bill of the servant.
We calculate the bone volume that must be sacrificed in order to insert an 'osseointegrated' implant (sic!). For a 5mm implant. in diameter and a length of 15 mm. the volume of lost or damaged bone is more than 500 mm. cubes. (in fact, considering the area that goes into necrosis around the implant, the diameter to be considered is 7 mm; therefore: 3.5 x 3.5 x 3.14 x 15 = 576.9 cubic mm).
This is also serious because the patient already presents himself with sometimes important bone deficits, which the surgeon should remedy.
In the Tramonte technique, on the contrary, most of the time the lanceolate drill is sufficient to insert an implant with insignificant bone loss. In fact, the lanceolate cutter compactly descends the bone fragments on the external wall of the tunnel that is being created and when the cutter is removed only a few rods adhere to it.
It is therefore useless for the surgeon who uses the buried implants to affirm that the bone is missing and that therefore it is necessary to resort to a graft, perhaps taking it from the cranial case, given that this site has the gold standard of success.
Limiting osteoplasty and non-essential detachments means respecting the patient.
Future implant health is linked to the shape of the implant and compliance with these rules.
The structure of the bone and its nutrition.
It should be remembered here that the intertwined meshes of the Havers and Wolkmann canals are not only elements of nutrition and growth, trophism and remodeling.
They are also essential structural constituents of the bone and guarantee the functionality of the relative apparatus through their strength, lightness and elasticity.
Let's imagine this three-dimensional network for a moment and think at how many points we have to interrupt these meshes in order to insert an implant.
It is intuitive that minimizing the number of interrupted links allows the healing processes to be faster and the structure of the mandible or maxilla to weaken as little as possible while retaining its ability to absorb chewing loads at best.
Considering these aspects of the problem is important because the mandibles receiving these interventions are most of the time already reabsorbed in varying degrees, in thickness, height, width, angle between the occlusal plane and the implant body, in the implant crown ratio and obviously in the bone density, as Mish rightly tells us.
But the presence of a flap separates the tissues that provide nutrition to the osteoblastic cells from the outer surface of the cortical bone.
The section of the perforating arteries involves necrosis of the osteocytes of the bone resulting in further hypotrophy of the bone itself and lengthening of the healing times. (8% of the jaws involved are still lost).
These comments are not free and I consider it very appropriate to take them into due account.
In a historical period in which all interventions are minimally invasive, contemporary dentistry prides itself on still very bloody techniques as if to emphasize its surgical dignity compared to more noble specialties.
But our patients do not need them and do not look for them, also because their age and their condition become more and more fragile.
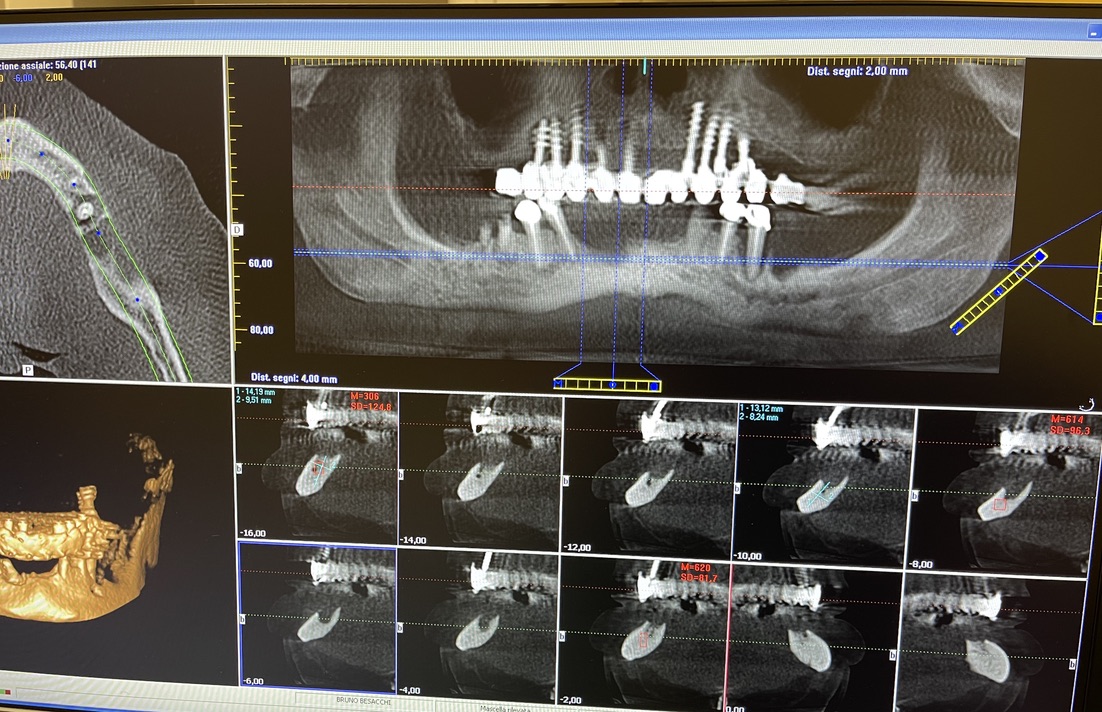
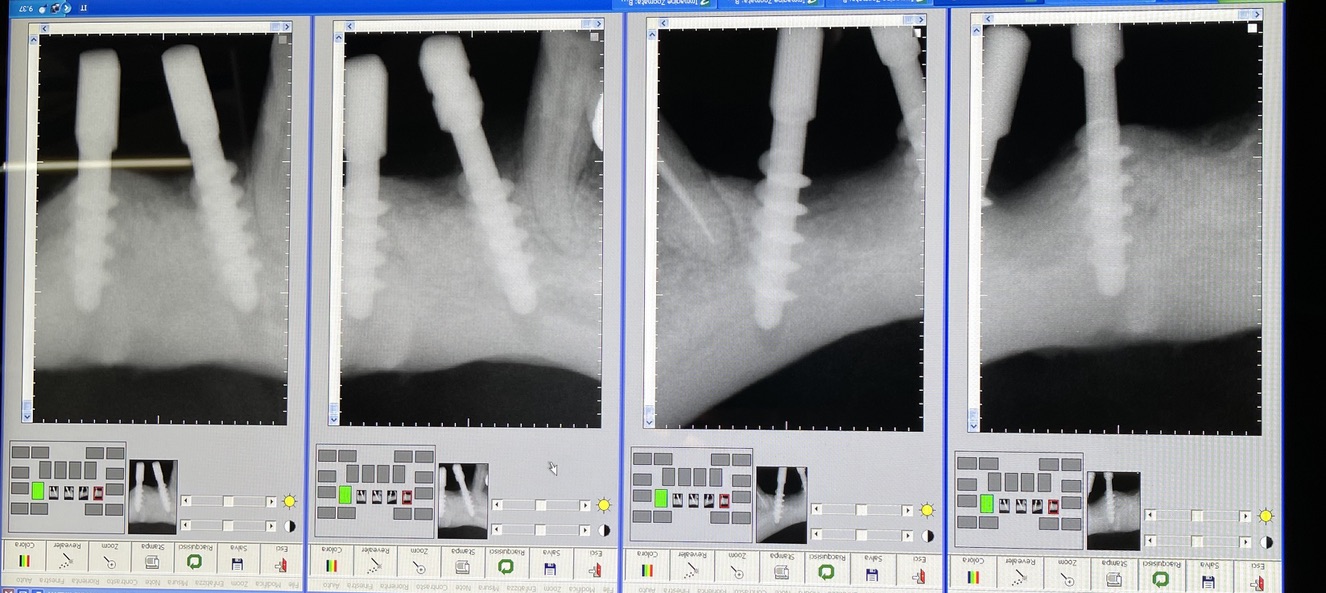
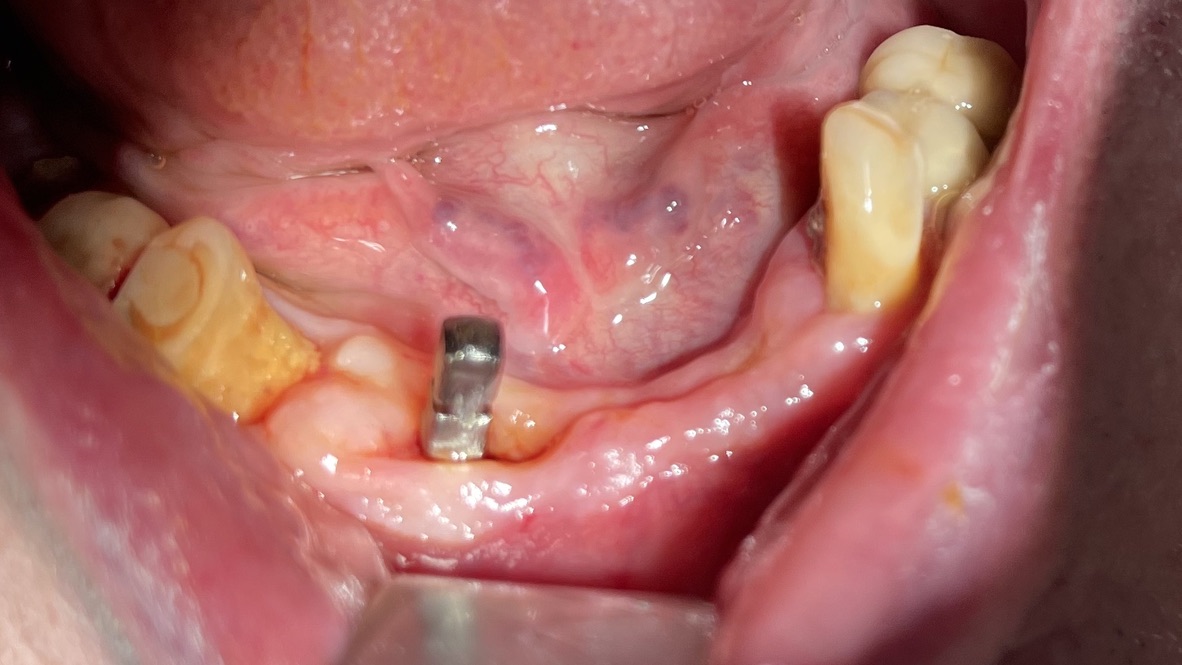
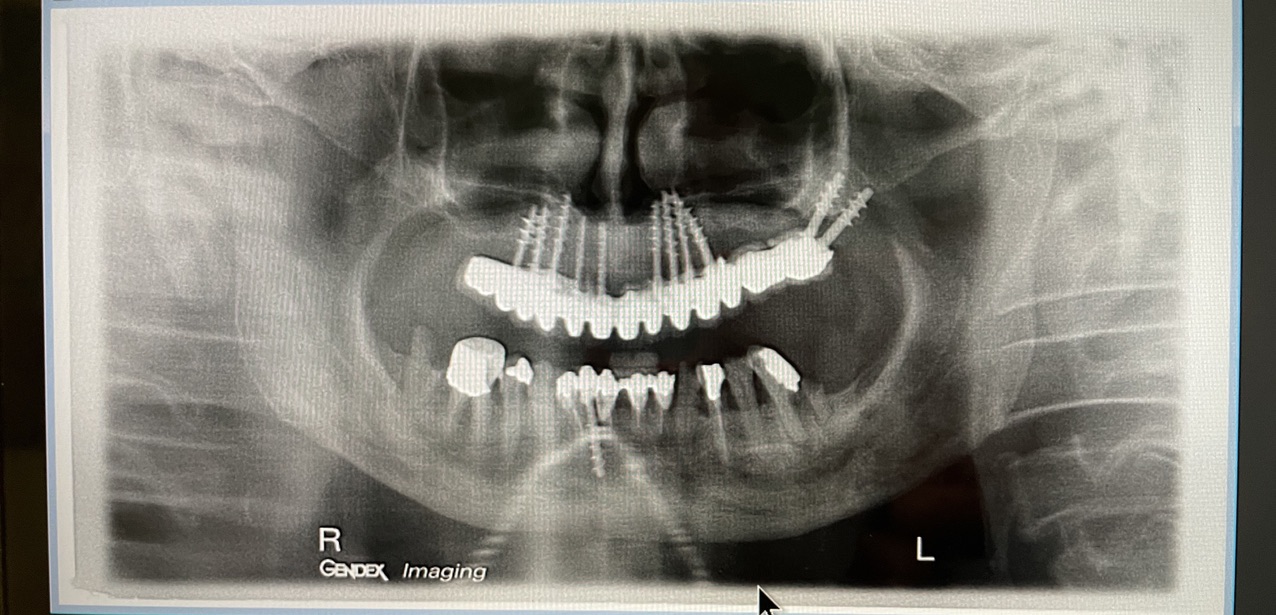
CLINICAL CASE combined with news n.6. Rehabilitation of 04/28/2021
In particular, I consider the following aspects to be significant:
- 1 Age of the patient: 83 years old
- 2 Execution of the first 6 plants: 25 years ago.
- 3 Execution of the 5 subsequent plants: 14 years ago
- 4 Medicines taken by the patient: none
- 5 Presence of implants in the tuber / pterygoid area
- 6 Presence of ancient inclined implants
- 7 Presence of implant bent in 25. (To parallelize it)
- 8 Presence of two mini-plants in 11-12
- 9 Presence of a welded bar in the upper sector
- 10 Severe periodontal disease of the lower sector
- 11 Hygiene issues
- 12 Implant failure of lower Tramonte implant, implant prior to 2004, in the context of general periodontal disease
- 13 The insertion of the three implants did not involve bone or connective tissue grafts
- 14 It did not make detachments necessary
- 15 It was not necessary to isolate the emergencies of the inferior alveolar nerves
- 16 Since we are dealing with high-density bone, we resorted to the helical drill, an instrument rarely used by us because it is not necessary and because there are areas where its use involves surgical risks that are not acceptable to us. In addition, this drill removes discrete amounts of bone that we prefer to remain where nature has put it. It is interesting that the diameter of the cutter is only 2 mm
- 17 Being dense bone, the implants used had a diameter of only 4 mm after tapping with the corresponding tap
- 18 At the check-up on 3/5/2021 the patient is not swollen and reports that he is finally eating well
- 19 Implant surgery starts at 8.45am. end of implant surgery at 9.36
- 20 Cementation of the provisional, packaged at the moment, completed at 10.30. total length of stay of the patient in the clinic 1.45 hours.
The images provide additional information in the captions.